
Imaging in PelvicInflammatory Disease:Ultrasound and CT
Mindy M. Horrow, MD, FACR, FAIUM
Director of Body Imaging
Albert Einstein Medical Center
Clinical Associate Professor of Radiology
Thomas Jefferson University School of Medicine
All photos retain the copyrights of their original owners
© Mindy Horrow, MD

Learning Objectives
Describe the variety of sonographicappearances of the abnormal fallopiantube in PID
Differentiate between findings of acuteand chronic PID by ultrasound
Describe the primary and secondaryfindings of PID on CT and how itcomplements ultrasound

Background
In 1990, costs of acute infection estimated at$4.24 billion with 200,000 hospitalizations and1,277,700 outpatients
Since then hospitalizations have decreased25% with slight increase in outpatient visits
Recent estimates are of 780,000 new cases ofacute PID annually
Study in 2004 found 4.2% incidence ofchlamydial infection in young adults
Cost of PID stems from chronic sequelae withaverage per person lifetime cost ranging from$1,060 to $3,180

Background
Chronic sequelae includeinfertility, ectopic pregnancy,chronic pelvic pain
Risk factors related to exposure toSTDs: earlier age first intercourse,multiple partners, prior STD,vaginal douche, race

Pathophysiology
Most cases caused by Neisseriagonorrhoeae and/or Chlamydia trachomatis
Other organisms: streptococcus, E. coli, H.influenza, Bacteroides, Peptostreptococcus
Initial lower genital infection which ifuntreated ascends into uterus, aided bycervical ectopy and menstruation (mucusplug expelled)
After transient endometritis, may causetubal inflammation with adhesions andobstruction, spread to peritoneum andovary

Diagnosis of PID
In 50% clinical sx are insufficient for dx
Combination of fever, severe pain,leukocytosis, ESR is specific but notsensitive
Clinical dx confirmed at laparoscopy inonly 67%
Endometrial bx has 90% sensitivity andspecificity compared to laparoscopy
Molander, Ultras ObGyn 17:233-238, 2001

Ultrasound
Frequently used, but no large trials ofsensitivity and specificity
Probably insensitive for mildabnormalities and non-specific for somefindings
Review of literature showssensitivity/specificity depends uponfindings considered to indicate PID,quality of equipment and imager.Trans-vaginal imaging most useful

Sonographic Findings: Subtle
Uterus- enlarged, fluid in endometrium,indistinct borders. Not very sensitive andoften difficult to appreciate
Free fluid- not a discriminatory finding insmall to moderate amounts
Ovaries- enlarged with multiple smallcysts (overlaps with normal ovaries)
Cacciatore, Obstet Gyn 80:912, 1992
Patten, JUM 9:681,1990



Sagittal uterus 6/16 6/23
Indistinct borders and EMS Normal definition




Sagittal 3/3 Transverse 3/3
3/7 3/7
Comparison of amount and appearance of fluid, ovarian
size and borders

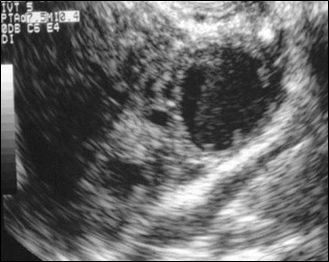
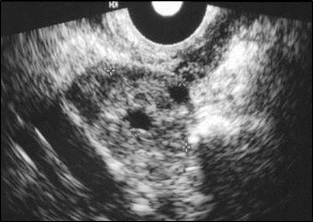
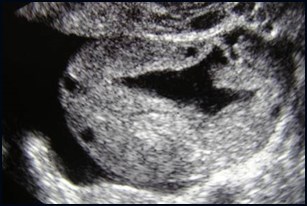
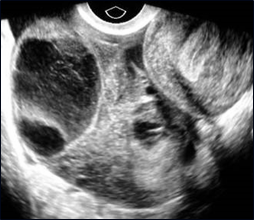
Polycystic-like ovaries
Multiple small cysts in an enlarged ovary
With endometrial bx proven plasma cellendometritis as marker for PID, 13/13(100%) with and 11/38 (29%) withoutpositive biopsy had polycystic ovaries, (P< .05)
Proposed mechanism- oophoritis causesinflammation and edema, increasingstroma and size and number of cysts
Cacciatore Obstet Gyn 1992; 80:912


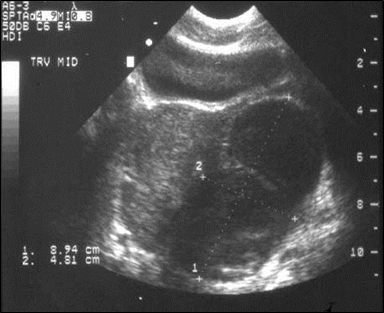
Volume of left ovary 28cc with adjacent
Thickened tube
tube

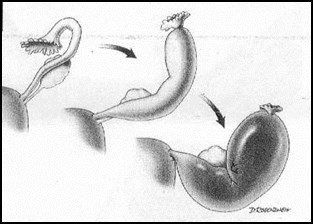
Fallopian Tubes
Sonographic demonstration of abnormaltube is hallmark of PID
Findings classified as acute or chronic
May involve ovary in complex or abscess
Acute salpingitis- mild dilatation, minimalif any fluid
Pyosalpinx or hydrosalpinx- moredilatation
Understanding types of abnormalitieshelps improve scanning

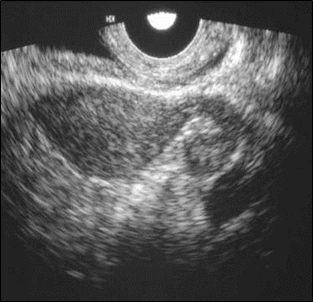
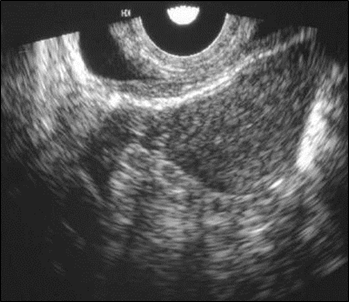
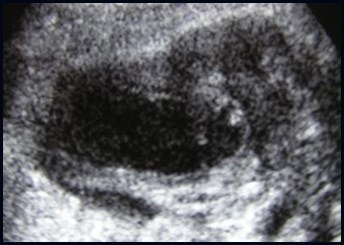
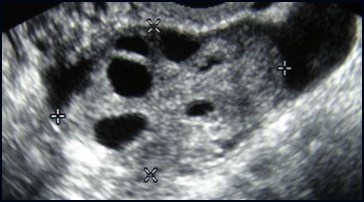
Fallopian Tubes
Best marker for acute or chronicsalpingitis is ovoid fluid filled structurewith incomplete septum- linear,echogenic protrusion arising from onewall but not reaching the opposite
Thick wall ( 5mm) and “cogwheel” signare best markers for acute disease
Thin wall (< 5mm) and “beads on string”indicates chronic disease
Other findings: tubular, “solid” structureseparate from ovary, fluid/debris level,gas
Timor-Tritsch Ultra Obstet Gyn 1998; 12:56

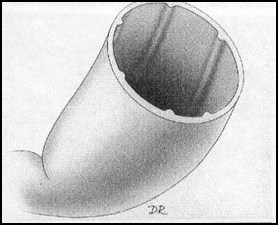
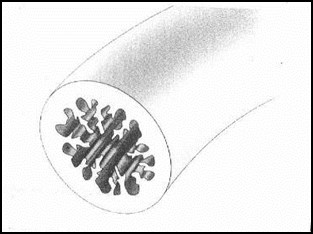
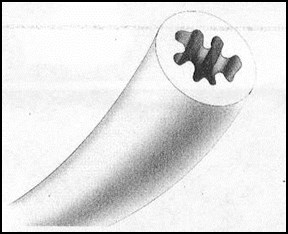
Normal tube “Cogwheel sign”
Kinked, fluid filled tube “Beads-on-string” sign
Timor-Tritsch Ultra Obstet Gyn 1998; 12:56


Normal Fallopian tube outlined by blood from rupturedhemorrhagic cyst

Elongated, solid tubular structures that are separatefrom ovaries. No incomplete septum or cogwheelsign because there is no fluid within tube
Acute Salpingitis
Molander, US Obstet Gyn 2001;17:233

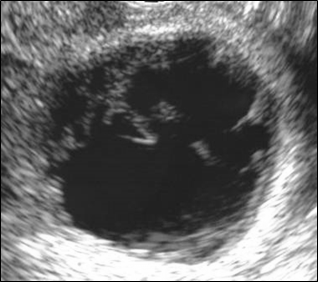
Incomplete Septum Sign
Tube distends and folds upon itself creating anincomplete “break” which appears as the septum
Chronic Acute



History of PID 8 years ago, now withchronic pain
Hydrosalpinx with “beads-on-string”
Coronal Sagittal
Ovary

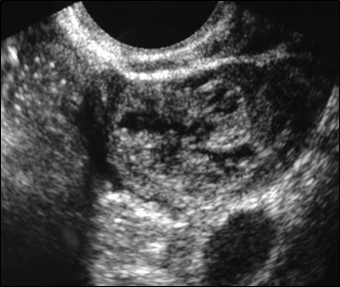
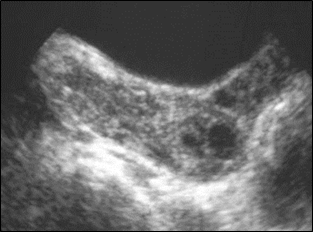
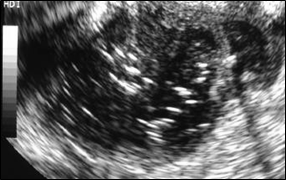
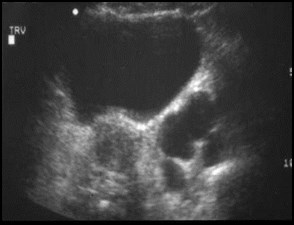
Examples of “Cogwheel Sign”
cross section of thick walled tube appears assonolucent wheel shaped structure
Acute salpingitis Pyosalpinx

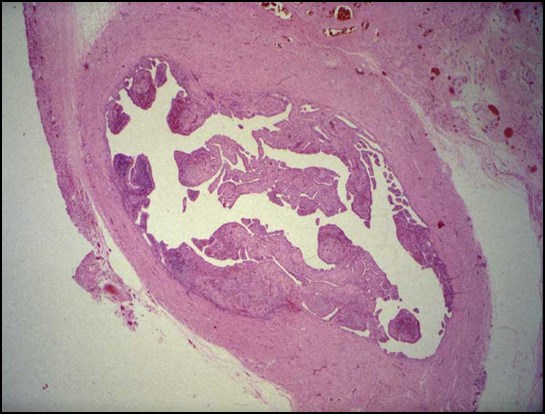
Path specimen demonstrating cogwheel sign


Coronal Sagittal
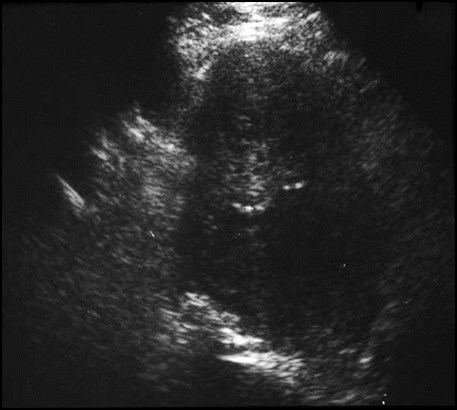
Thick walled tubular structure with fluid/debris level =pyosalpinx




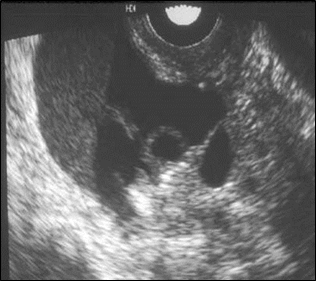
Bilateral Pyosalpinges
Left
Right

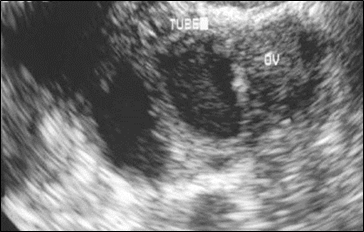
Tubo-ovarian complex: occluded, inflamed tubeadheres to ovary
O
O

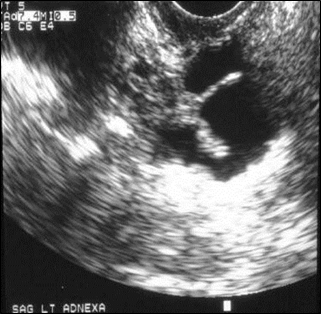
Tubo-ovarian Abscess
Acutely ill patient with marked tenderness, Conglomerate oftissues in which separate tube and ovary cannot bedistinguished




Bilateral tubo-ovarian abscesses with gas
Right Left


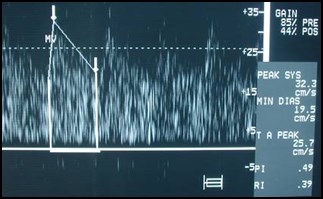
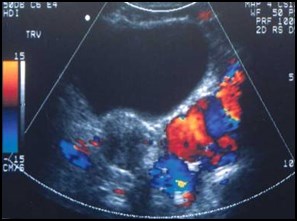
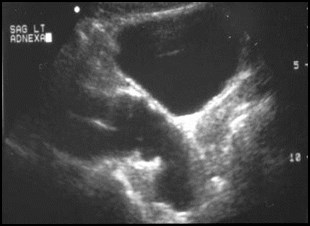
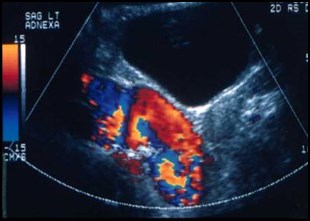
Doppler in PID
In acute PID, generalized hyperemia with lowresistance flow, though PI and RI overlap withchronic PID
Molander, US Obstet Gyn 2001; 17:233
Tepper, J Clin US 1998; 26:247

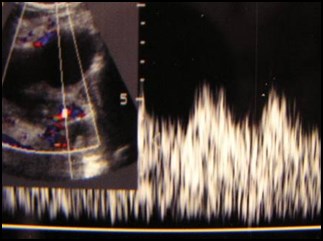
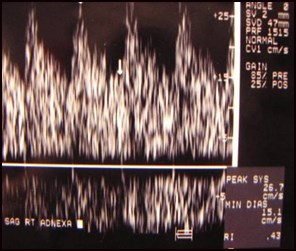
Increased color Doppler with low resistanceindicates acute PID with pyosalpinx



Chronic right pelvic pain, history of PID
Sag ROV
Trv ovaries
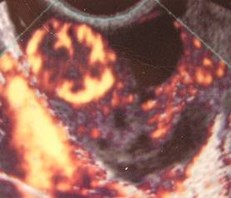
PeritonealInclusion Cyst

Sonography of PID with Tx
Complex fluid and inflammation canresolve in a few days.
Pyosalpinx can change to hydrosalpinxand possibly resolve over few weeks tomonths
Study of Taipale,etal found 9 of 55 pts withclinical PID and initial normal sonogramdeveloped a hydrosalpinx over time.
If a pyosalpinx does not resolve ordevelops into a hydrosalpinx, probablysignifies an incompletely treated infection
Taipale, etal US Obstet Gynecol. 1995;6;430

CT Findings in Acute PID
Early: thickening of utero-sacralligaments, haziness of pelvic fat.Thickened tubes, enlarged enhancingovaries, increased endometrialenhancement with fluid
Advanced: Pyosalpinx, tubo-ovarianabscess
Adjacent structures: ileus,hydonephrosis, Fitz-Hugh-Curtissyndrome (inflammation of right upperquadrant)

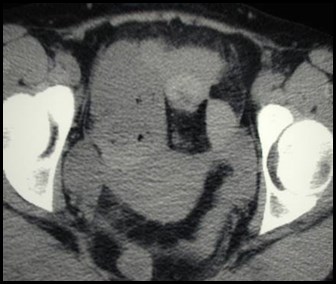
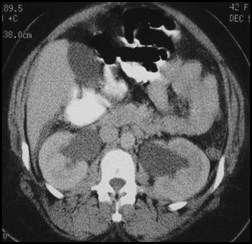
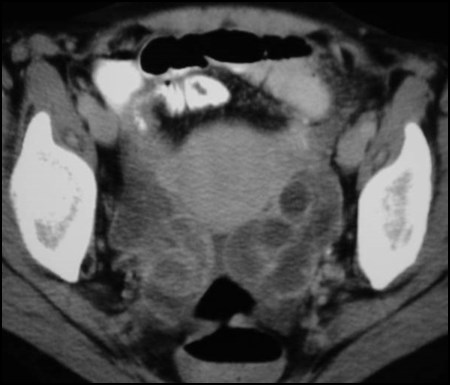
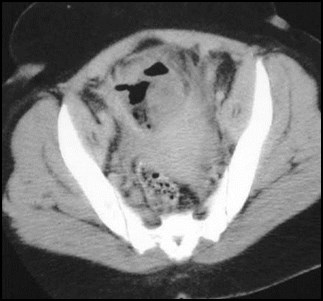
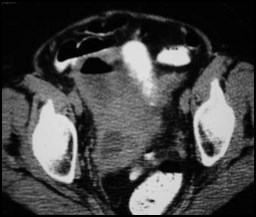
25 year old with fever, wbc= 40,000, acute renalfailure and signs of peritonitis
Only abnormality on CT: haziness of fat in pelvis
Surgery revealed PID

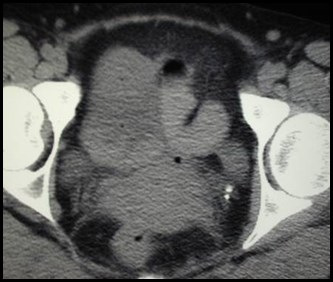
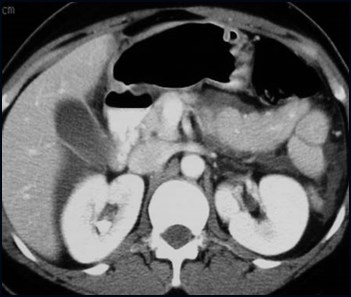
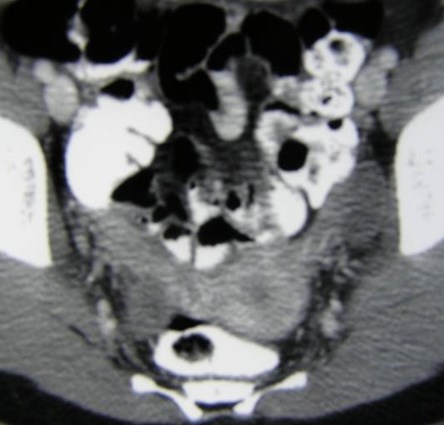
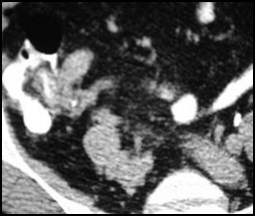
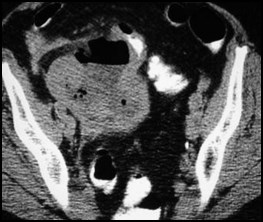
CT in patient with left flank pain and possible pyelonephritis
Enlarged ovaries due to oophoritis and peritonealinflammation extending along left flank, normal kidneys



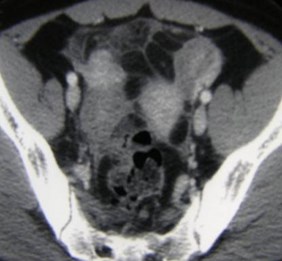
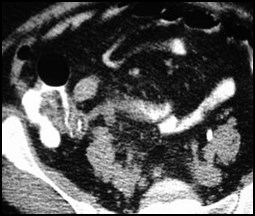
Hazy fat, hydronephrosis, TOAs, fluid, ileus


Inflammation and bilateral tubo-ovarianabnormalities



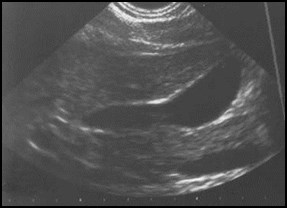
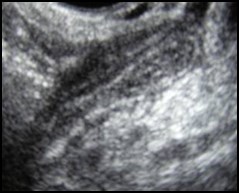
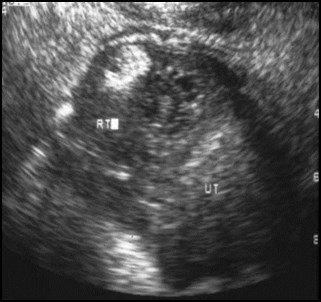
Trans-abdominal and trans-vaginal images in same patient
Increased prominence and echogenicity of surroundingfat on ultrasound corresponds to hazy pelvic fat on CT



Bilateral tubo-ovarian complexes
T
T

Fitz-Hugh Curtis Syndrome
Right upper quadrant pain and “perihepatitis”associated with PID
Thickening of right anterior pararenal space onultrasound. (9 cases)
Enhancement of anterior surface of liver on CT(single case)
Pericholecystic inflammation and transienthepatic perfusion abnormality on CT (singlecase)
Schoenfeld, JCU 1992; 20:339
Tsubuku, JCAT 2002; 26:456
Pickhardt, AJR 2003; 180:1605

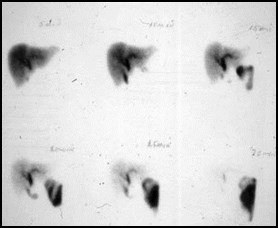


Delayed GB visualization
At three hours
Normal gallbladder US
PID on pelvic US


Acute right sidedabdominal pain
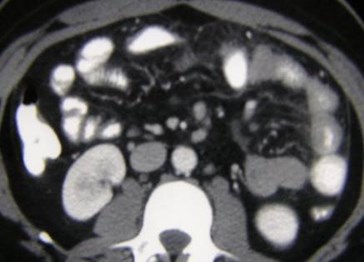
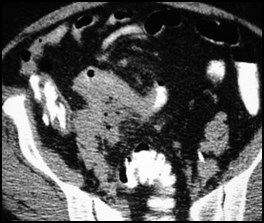
Fluid in Morrison’s pouch and around the liver, hyperenhancement of gallbladder wall

Bilateral pyosalpinges
PID with FHC Syndrome

PID “Look-a-likes”
Alternative diagnoses

Right lower quadrant pain
Pyosalpinx vs. Appendicitis
Tube orappendix?



Uterus
Appendicitis

Appendiceal Abscess

63 year old woman with right lower quadrantpain and elevated white blood cell count


Perforated Appendicitis with right pyosalpinx and pyometra

Non-pregnant patient with left lower quadrant pain,interpreted as dilated left tube with free fluid c/w PID
L R
Ruptured left corpus luteal cyst




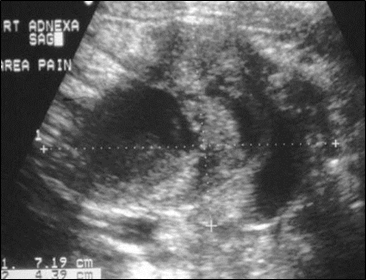
Right adnexal pain, no fever or wbc
Ruptured Hemorrhagic Cyst

37 year old with IUD and left sided paindiagnosed as TOA and treated medically
April
U



Returned in August with pus draining from skin
Diverticular abscess with
colo-cutaneous fistula

Transverse Sagittal


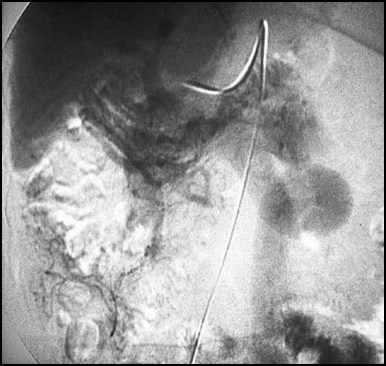
Pelvic varices in patient with portal HTN
Pelvic varices to IMV IMV to portal vein
Portal phase images from SMA injection

Conclusions
Use transvaginal ultrasound as primaryimaging modality, sometimes withtransabdominal for overview of pelvis andto evaluate for associated abnormalities.Doppler of limited help.
Be aware of variety of appearances ofabnormal fallopian tubes in both acute andchronic PID. Careful scanning will allow oneto make specific diagnosis (salpingitis,pyosalpinx, etc.)
Tukeva, etal. Radiology 1999;210:209)

CT ordered more frequently because ofincreased use in ER for abdominal pain. Ifthere is no specific abnormality, but justgeneralized haziness of pelvic fat andthickening of ligaments, think PID
? Use of MR
Tukeva, etal. Radiology 1999;210:209)
Conclusions

The End